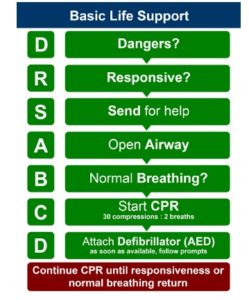
DRSABCD
In any First Aid course you will no doubt have come across the acronym DRSABCD many times, but it’s important to remember, that’s all it is, an acronym.
The DRSABCD acronym represents the chain of events, actions and decision making when treating a person who suddenly loses consciousness.
Of course, these scenarios may range in severity from something very minor through to something life threatening and potentially fatal.
DRSABCD – what does it mean ?
First of all, the DRSABCD acronym can be used for 2 entirely different situations.
DRABCD when Casualty is Unconscious & NOT breathing
Danger
– always check the danger to you, any bystanders and then the injured or ill person. You need to try and identify any potential hazard which will affect your ability to safely manage the casualty.
Dangers generally fall into one of the following categories:
- Manual handling
- Risk of Infection
- Environment (e.g. fire, electricity, traffic).
Response
– is the person conscious? Do they respond when you talk to them, touch their hands or squeeze their shoulder?
If there is a response:
- make them comfortable
- check for injuries
- monitor their response.
Assess for signs of life. Lack of movement, unconsciousness, lack of breathing or abnormal breathing may indicate no signs of life.
A person that gives no response or only a minimal response (e.g. groaning without opening their eyes) should be treated as unconscious.
Unconsciousness may be caused by:
- Low brain oxygen levels
- Heart and circulation issues (e.g. fainting, arrhythmia)
- Metabolic issues (e.g. overdose, intoxication, hypoglycaemia)
- Brain issues (e.g. head injury, stroke, tumour, epilepsy).
If there is no response…
Send for Help
– call triple zero (000). Don’t forget to answer the questions asked by the operator.
If you are not alone, delegate someone to call emergency services and retrieve an AED if possible.
Airways
– Is the person’s airway clear? Is the person breathing?
Managing the patient/resident’s airway must take priority over any other injury they have, including a spinal injury
Open airway by tilting head with chin lift.
If an unconscious patient/resident is lying on their back, their tongue may fall against the back wall of their throat and obstruct airflow
Other potential causes of airway obstruction include:
- Semi-solid material (e.g. vomit, seaweed)
- Solid material in the airway entrance or within the upper airway
- Laryngeal spasm (a reflexive closure of the trachea entrance in response to foreign matter irritating the vocal cords)
- Swelling from asthma, allergies etc.
- Injuries involving the airway (e.g. from smoke, toxic fumes).
If foreign material is present:
- place patient in recovery position
- Clear the patient/resident’s airway by opening their mouth and turning their head slightly downwards. This will allow foreign material such as food, vomit, blood and secretions to drain. You may use a finger sweep to manually remove foreign bodies
Breathing
– When assessing the patient/resident’s breathing:
- Look for upper abdomen or chest movement
- Listen for air escaping from the nose and mouth
- Feel for air movement at the nose and mouth.
If the patient/resident is unresponsive and gasping or breathing abnormally, they require resuscitation. Abnormal breathing may be caused by:
- Depression of or damage to the respiratory center in the brain
- Upper airway obstruction
- Paralysis or impairment of the nerves and/or muscles required for breathing
- Lung problems
- Drowning
- Suffocation.
Palpation of a pulse is unreliable and should not be performed to confirm the need for
resuscitation
Compressions (or CPR)
– if an adult is unconscious and not breathing, make sure they are flat on their back and then place the heel of one hand in the center of their chest and your other hand on top. Press down firmly and smoothly (compressing to one third of their chest depth) 30 times. Give two breaths.
- Chest compressions should be performed at a rate of 100 to 120 bpm (beats per minute) (about 2 per second) regardless of age.
To get the breath in, tilt their head back gently by lifting their chin. Seal their nostrils closed, place your open mouth firmly over their open mouth and blow firmly into their mouth to inflate the lungs.
If the chest does not rise this may indicate obstruction or improper technique (not enough air being blown into the lungs or inadequate air seal around the patient/resident’s mouth and nose
Consider using a barrier device if one is available. However, risk of disease transmission through rescue breaths is low so do not be deterred if a barrier device is unavailable.
Keep going with the 30 compressions and two breaths at the speed of approximately five cycles in two minutes.
Start CPR: 30 chest compressions followed by 2 breaths.
Continue CPR until help arrives or patient recovers.
Defibrillation
– for unconscious adults who are not breathing, apply an automated external defibrillator (AED) if one is available. An AED is a machine that delivers an electrical shock to cancel any irregular heart beat (arrhythmia), in an effort get the normal heart beating to re-establish itself.
CPR should be performed until an AED is retrieved, turned on and attached.
The devices are very simple to operate. Just follow the instructions and pictures on the machine, and on the package of the pads, as well as the voice prompts. If the person responds to defibrillation, turn them onto their side and tilt their head to maintain their airway.
Proper pad placement is crucial to ensure the shock is delivered on an axis through the heart. Place one pad just below the collarbone on the patient/resident’s right chest and the second below the patient/resident’s left armpit.
Anterior-posterior electrode placement may be considered if defibrillation electrodes are at risk of overlapping (eg small children)
It is your responsibility to know the location of AEDs in your workplace or club.
AEDs must only be used in conjunction with CPR
If the defibrillation is successful, the patient/resident will have a return of spontaneous circulation (ROSC), become responsive and start to breathe independently. You should:
- Stop CPR
- Leave the AED pads attached (in case the patient/resident goes back into arrest)
- Closely monitor the patient/resident
- Place the patient/resident in the left lateral (recovery) position
- Wait for help to arrive.
DRABCD when Casualty is Unconscious but IS breathing
All DRSABCD steps are the same as above, except, as noted below
Danger
Response
Send for Help
Airways
Breathing
If the person is unconscious but breathing normally, turn them onto their side, carefully ensuring that you keep their head, neck and spine in alignment. Monitor their breathing until you hand over to the ambulance officers.
If the patient’s breathing is normal:
- place patient in recovery position
- monitor breathing
- manage injuries
- treat for shock.
CPR Is not required in this instance.
Circulation
Check pulse to determine whether casualty is in shock
Signs of shock can include:
- weak, rapid pulse
- cold, clammy skin
- faintness/dizziness
- nausea.
Dangerous/Deadly Bleeding
Promptly control any bleeding, particularly arterial bleeding. Apply firm direct pressure.
For non-arterial bleeds, Place a sterile bandage or clean cloth on the wound. Press the bandage firmly with your palm to control bleeding. Apply constant pressure until the bleeding stops.
Maintain pressure by binding the wound with a thick bandage or a piece of clean cloth.
Global Fitness Institute conducts First Aid Courses under the trading name, First Aid Oz.
Units we deliver include:
- HLTAID011 Provide First Aid
- HLTAID014 Provide Advanced First Aid
- HLTAID009 Provide Cardiopulmonary Resuscitation
- HLTAID012 Provide an emergency FirstAid response in an Education and Care setting
- PUAOPE010 Operate an Automated External Defibrillator in an emergency
For all our First Aid course options and upcoming course dates, visit First Aid Oz